May 22, 2023
Wilma Peterson Cross, M.S.
Deputy Director, Office of Disease Prevention
6705 Rockledge Drive, Room 733 MSC 7990 Bethesda, MD 20892 USA
Re: National Institute of Health Office of Disease Prevention Request for Information on the NIH Office of Disease Prevention Strategic Plan for Fiscal Years 2024 - 2028.
via website: https://rfi.grants.nih.gov/?s=63d9edb46e8d6ea804099132
The American Association for Dental, Oral, and Craniofacial Research (AADOCR) is the leading professional community for multidisciplinary scientists who advance dental, oral, and craniofacial research. We appreciate the opportunity to share our thoughts on the request for information on the Office of Disease Prevention (ODP) strategic plan for fiscal years 2024 – 2028. AADOCR recognizes and applauds the ODP’s efforts toward assessing, facilitating, and stimulating research in disease prevention, and disseminating the results of this research to improve public health. To respond to this request for comments, AADOCR engaged its Science Information Committee and its Board of Directors.
Systematically monitor NIH investments in prevention research and the progress and results of that research
- Objective 1.3: Partner with NIH Institutes, Centers, and Offices and other federal agencies to disseminate ODP portfolio analysis tools and related data.
Oral health is a key indicator of general health, well-being, and quality of life, while at the same time sharing modifiable risk factors with some of the most prevalent non-communicable diseases - cardiovascular diseases (CVD), cancer, diabetes, and chronic respiratory diseases. Oral diseases are among the most common NCDs worldwide, affecting an estimated 3.5 billion people1 – representing more than half of the global population. The combined estimated number of cases of oral diseases globally is about 1 billion higher than the combined number from all five main NCDs2. As of 2019, the most prevalent oral diseases/conditions were untreated dental caries (2.5 billion cases), severe periodontal disease (1 billion cases), and edentulism (350 million cases)1. It is therefore important that we take a preventative approach that includes the dissemination and implementation of results from preventative research related to oral diseases. AADOCR supports close collaboration and coordination between the ODP and the National Institutes of Dental and Craniofacial Research (NIDCR) to disseminate ODP portfolio analysis tools and related data and to coordinate of funding initiatives related to oral disease prevention.
Identify prevention research areas for investment or expanded effort by NIH.
- Objective 2.1: Work with a variety of partners to identify needs in prevention research.
- Objective 2.3: Work across ODP and with NIH Institutes, Centers, and Offices and other partners to identify the most promising/feasible prevention research gaps that warrant greater investment or expanded effort.
As mentioned earlier, AADOCR is the leading professional community for multidisciplinary scientists who advance dental, oral, and craniofacial research. AADOCR is well positioned to support and represent the dental, oral, and craniofacial research community, provide scientific career development, increase opportunities for scientific exchange, advance prevention science research related to dental, oral, and craniofacial health, and facilitate the application of research findings. The International Association for Dental Research’s (IADR) scientific groups and networks are the backbone of the association. Comprised of 25 scientific groups and 10 networks, these communities bring colleagues across disciplines together to inspire and promote high-quality research in a wide breadth of DOC scientific areas. Therefore, AADOCR is primed to work with ODP and the NIDCR to discern further prevention research areas for investment or expanded effort by the NIH that is inclusive of dental, oral, and craniofacial research.
- Objective 2.2: Compare identified needs in prevention research with the current NIH portfolio to identify prevention research gaps (i.e., those areas that are not being addressed or have insufficient funding).
There is research – over 7 decades’ worth – pointing to the safety and effectiveness of fluoride to prevent tooth decay. Dental caries (tooth decay) remains the most prevalent chronic disease in both adults and children and fluoridated water is a simple, equitable, and effective strategy that can help millions of people3,4 However, there have been frequent and persistent challenges to water fluoridation. Therefore, AADOCR supports research on water fluoridation to continue to confirm its safety and effectiveness, in the current context of fluoride availability and within optimal levels. Research is needed that further demonstrates the safety of the low fluoride exposure concentrations (less than 1.5 mg/L), including those in fluoridated drinking water, and examining total fluoride exposure. There has been a trend of people drinking more non-fluoridated bottled water instead of community fluoridated tap water5. More research is also needed to better understand if fluoride dietary supplements and fluoridated water help improve bone health and prevent fractures. Additionally, more research is needed to further demonstrate the positive impact of fluoride in different delivery systems and community water fluoridation on reducing oral health disparities amongst children as well as across the lifespan.
Advance tobacco regulatory and prevention science.
- Objective 5.5: Facilitate development of resources and research opportunities to address gaps in tobacco prevention intervention, research, measurement, and methodology.
AADOCR recognizes that tobacco use is one of the largest public health threats in the world6. Reports show that most people who use cigarettes began smoking as an adolescent7; and nearly nine out of 10 smokers started smoking by age 187. Additionally, since 2014, electronic nicotine delivery systems (ENDS), specifically e-cigarettes, have been the most commonly used tobacco-derived product among U.S. youth8. In 2022, about 1 in 10 (2.5 million) U.S. middle and high school students reported current e-cigarette use9. Adolescents who use e-cigarettes are 3.5 times more likely to report using traditional cigarettes and 4 times more likely to continue their use past 30 days10. Therefore, AADOCR supports the development of research opportunities that foster more behavioral studies that discern effective mechanisms to prevent adolescents from acquiring a nicotine habit. In addition to the health consequences for the ENDS user, the effects of the exhaled aerosols on others are also a concern. Further research is needed on the health effects of secondary exposure to ENDS aerosols.
Promote and coordinate prevention research that addresses health disparities.
- Objective 6.2: Assess the NIH prevention research portfolio related to health disparities to identify research, infrastructure, and training gaps and develop strategies to address those gaps.
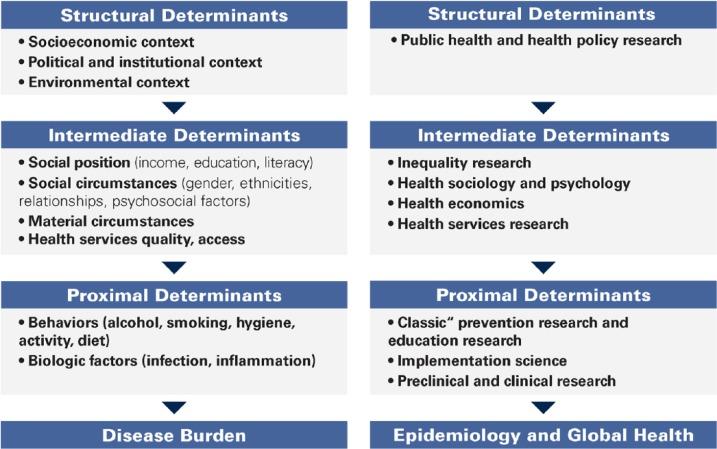
Figure 1 The pathway to (unfair) disease distribution (left) and research levels (right) suited to address the underlying structural or procedural causes (Schwendicke et al). |
Access to dental care is limited for higher-need / lower-income populations where major social gradients exist11. Prevention is mainly delivered in the dental chair, which perpetuates the problems of the interventionist care model - the dentist is responsible for “delivering” prevention; patients are “consumers” rather than participants in this preventive approach12. The current model of dental care and the conventional focus of “preventive dentistry” unfortunately targets only a fraction of the structural and procedural causes leading to existing oral health inequalities (figure 1)11. Therefore, widespread dental prevention efforts need to examine the myriad causes of the lack of penetration of prevention to broad patient populations where access to dental care is limited. AADOCR supports further prevention research that examines the varied determinants that continue to perpetuate the systemic inequities in oral health care and diseases. It is important to note that this area of research requires a lot of interdisciplinary collaborative work and community engagement. Collaboration is needed across agencies with multiple institutional funding streams.
Improve the availability and visibility of information about prevention research, inform diverse audiences about the scope and impact of disease prevention research, and engage with ODP’s partners to enhance and support ODP’s mission.
- Objective 7.1: Improve the availability and visibility of information about prevention research and promote prevention-related events conducted by NIH and other federal agencies.
Progress in dentistry is often defined along technological advances facilitating reconstructive procedures, while the biological underpinnings are not as well aligned6. Many dental practitioners focus on treating the symptoms of oral diseases versus emphasizing prevention and prevention research. This clinical paradigm stems from existing dental educational models with a greater emphasis in some schools on the technical principles without similar attention paid to the prevention of disease and how it can be applied in the dental practice setting6. Therefore, AADOCR supports working closely with dental school deans to disseminate and transfer knowledge gained from prevention research with their students and residents and integrate this knowledge into their educational curricula. It would also be beneficial to extend this knowledge transfer to educational programs in the community/ K-12 level of school curriculum to improve health literacy and positive health behaviors.
AADOCR appreciates the opportunity to provide comments on the request for information on the NIH ODP strategic plan for fiscal years 2024 – 2028. AADOCR stands ready to work with ODP to flesh out prevention research gaps in dental, oral, and craniofacial sciences and mechanisms through which ODP can increase the dissemination of the data obtained.
If you have any further questions, please contact Dr. Makyba Charles-Ayinde, Director of Science Policy, at @email.
Sincerely,
|
1World Health Organization. (2022). Global Oral Health Status Report: Towards Universal Health Coverage for Oral Health by 2030. Retrieved from: https://www.who.int/team/noncommunicable-diseases/global-status-report-on-oral-health-2022. Accessed on May 18, 2023.
2Institute of Health Metrics and Evaluation. (2020). Global Burden of Disease 2019 Results [Online Database]. Retrieved from: https://vizhub.healthdata.org/gbd-results/. Accessed May 18, 2023.
ature Portfolio. (2022). Fees for Publishing in an “Open Choice” Journal. Retrieved from: https://support.nature.com/en/support/solutions/articles/6000137677-fees-for-publishing-in-an-open-choice-journal.
3International Association for Dental Research. (2022). Position Statement on Community Water Fluoridation. Retrieved from: https://www.iadr.org/science-policy/position-statement-community-water-fluoridation. Accessed on May 18, 2023.
4Centers for Disease Control and Prevention. (2021). Disparities in Oral Health. Retrieved from: https://www.cdc.gov/oralhealth/oral_health_disparities/index.htm. Accessed on May 18, 2023.
5Victory, K.R., Wilson, A.M., Cabrera, N.L. et al. Risk perceptions of drinking bottled vs. tap water in a low-income community on the US-Mexico Border. BMC Public Health 22, 1712 (2022). https://doi.org/10.1186/s12889-022-14109-5.
6American Association for Dental, Oral, and Craniofacial Research. (2023). Tobacco. Retrieved from: https://www.aadocr.org/science-policy/tobacco. Accessed on May 18, 2023.
7Centers for Disease Control and Prevention. (2022). Smoking and Tobacco Use: Youth and Tobacco Use. Reviewed 2022. Retrieved from: https://www.cdc.gov/tobacco/data_statistics/fact_sheets/youth_data/tobacco_use/index.htm. Accessed May 18, 2023.
8Food and Drug Administration. (2022). Results from the Annual National Youth Tobacco Survey: 2021 Findings on Youth Tobacco Use. Retrieved from: https://www.fda.gov/tobacco-products/youth-and-tobacco/results-annual-national-youth-tobacco-survey. Accessed May 18, 2023.
9Cooper M, Park-Lee E, Ren C, Cornelius M, Jamal A, Cullen KA. (2022). Notes from the Field: E-cigarette Use Among Middle and High School Students — United States, 2022. MMWR Morb Mortal Wkly Rep. 71:1283–1285.
10Soneji S, Barrington-Trimis JL, Wills TA, Leventhal AM, Unger JB, Gibson LA, Yang J, Primack BA, Andrews JA, Miech RA, Spindle TR, Dick DM, Eissenberg T, Hornik RC, Dang R, and Sargent JD. (2017).
11Association Between Initial Use of e-Cigarettes and Subsequent Cigarette Smoking Among Adolescents and Young Adults: A Systematic Review and Meta-analysis. JAMA Pediatr. 171(8):788-797.Schwendicke F, Giannobile WV. (2020). Research for Prevention of Oral/Dental Diseases: How Far Have We Come? J Dent Res. 99(1):5-7.
12Giannobile WV, Kornman KS, Williams RC. (2013). Personalized Medicine Enters Dentistry: What Might This Mean for Clinical Practice? J Am Dent Assoc. 144(8):874–876..